By Chuck Stadler, Jr – President and CEO of rtNOW.
One of my nursing instructors/mentors (Mona White) told me years ago, “The gauge of a great nurse is not to know everything, rather to know what questions to ask and where to find the answer”. Nobody can be comfortable and knowledgeable with every aspect of nursing, and anyone who claims to be is crazy. Nurses have all been taught to lean on their clinical peers for guidance. A respiratory therapist has always been a pivotal member of the clinical team, offering specialized respiratory expertise.
Using Minnesota as an example state1, in urban areas 1 respiratory therapist has the potential to serve 2,647 patients. In small rural towns, the ratio is 1 respiratory therapist to 5,746 patients. On the far end of the spectrum, in isolated rural areas the gap widens to an enormous 1 therapist to 29,143 patients. During the 2018 – 2019 data collection period a projected 104 openings across the state with a supply of 81 graduates to fill these openings2.
This is one example of respiratory therapist shortages that continue nationwide. They are a problematic reality in today’s healthcare landscape, but current technology can also provide an answer.
PDPM provides a unique opportunity for skilled nursing facilities to grow their respiratory resources through telerespiratory care while capturing PDPM dollars.
Whether you have partial respiratory coverage or no coverage at all, telerespiratory care is emerging as a viable way to increase the number of medically complex patients your staff can successfully handle, while capturing PDPM dollars. Nurses can quickly connect with a respiratory therapist via phone and video chat, who can then consult on equipment, perform respiratory assessments, make recommendations for treatment plans (i.e. NIV, CPAP, trach care), and serve as a supportive bedside resource to nurses, providers, and patients/residents. Once telerespiratory is integrated into a culture, experience has shown that it can be key to avoiding transfers. For examples of this, look at these case studies from rtNOW.
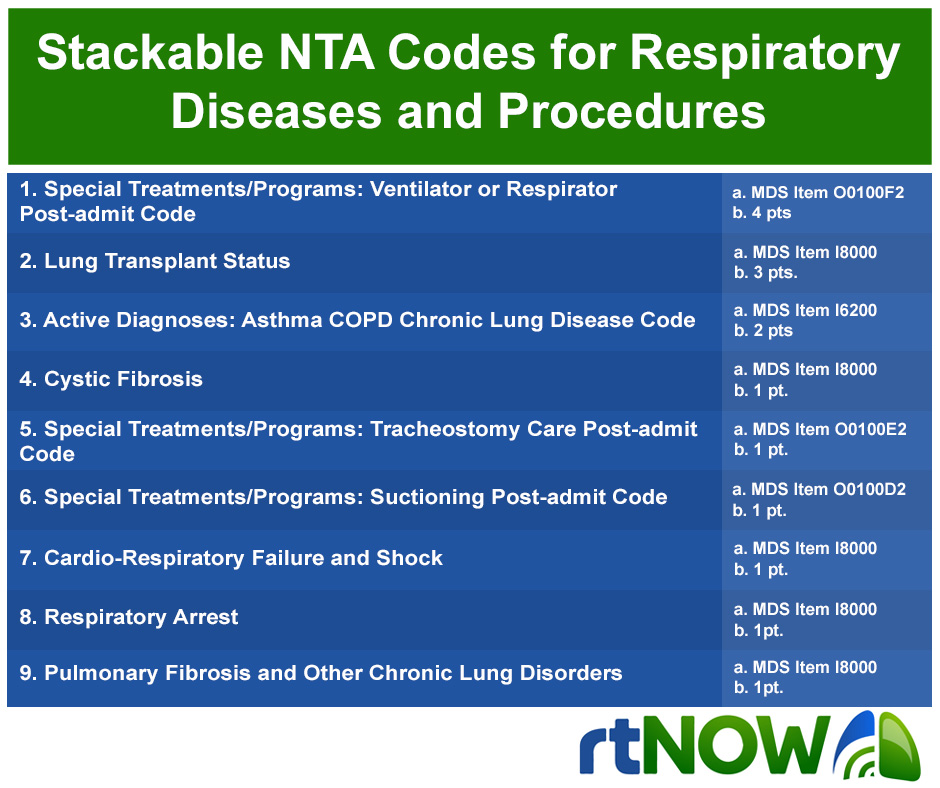
And the good news is that it makes financial sense. For all the change that is happening there are 9 stackable NTA codes3 specific for patients with respiratory comorbidities (Chart 1). As you know, there are many other codes that would be also associated with some of these patients with multiple comorbidities. PDPM provides a unique opportunity for skilled nursing facilities to grow their respiratory resources via telerespiratory care while capturing PDPM dollars.
If your organization is planning to take on the medically complex population, you will start to get pressure from all sides on how to care for them properly. It may be that your organization has been fortunate in finding and maintaining a respiratory therapist on day shifts, but what about the nights? Your evening/night shift clinical team probably has less experience and different staffing ratios than the day shift. Who are evening/night shift team supposed to use for guidance through the night? The administrator? DON, ADON? Will they wake up one of your day shift RT’s? Or will they continue to transfer the patient to the hospital? These are important questions, and thankfully we now have an answer.
I would like to propose that an easy solution is to give them a team of licensed RRT’s available with the touch of a button via telerespiratory. Pricing packages range between $4-5/hr depending on the amount of coverage desired. A small price to pay to add a knowledgeable team member at the immediate time and place your staff has a need.
References:
- Minnesota Department of Health: Office of Rural Health and Primary Care report on Minnesota’s Respiratory Therapist Workforce, 2016: https://www.health.state.mn.us/data/workforce/rt/docs/2016rtb.pdf
- Minnesota State Careerwise: https://careerwise.minnstate.edu/lmiwise/demand?id=OPS025&area=000000&ord=1
- CMS Website: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/Downloads/PDPM_Fact_Sheet_NTAComorbidityScoring_v2_508.pdf
